In cancers with peritoneal spread, the response to intravenous chemotherapy is limited or poor. There are various reasons for this:
- The barrier between the blood and the peritoneum (plasma-peritoneal barrier)
- Poor blood supply to the peritoneum
- Poor oxygenation of cancer cells
- Weak apoptosis (cell death) potential in hypoxic (low oxygen) tumor cells
- Diffuse inflammatory reaction surrounding tumor cells
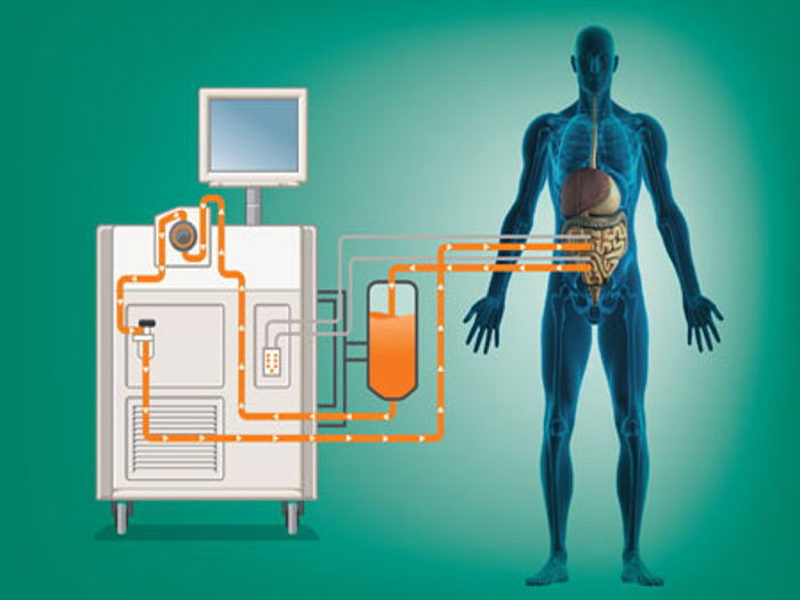
For these reasons, intravenous drugs have difficulty to reach tumors in the peritoneum and their effectiveness decreases. In particular, due to the plasma-peritoneal barrier, drugs can only reach the peritoneum in small amounts and reach the bone marrow and other organs in much higher amounts. This leads to decreased efficacy against the tumor and increased side effects. For this reason, intra-peritoneal chemotherapy was considered for cancers that have spread to the peritoneum and the method of cytoreduction + hyperthermic intraperitoneal chemotherapy (CRS-HIPEC) was introduced. Cytoreduction means the removal of all tumor foci that have spread to the peritoneum during surgery. Hyperthermic intraperitoneal chemotherapy is popularly known as 'hot chemotherapy'. Chemotherapy drug in about 4 liters of liquid is administered into the abdominal cavity at 41-42 degrees for 60-90 minutes.
Hyperthermia is thought to increase the effect of chemotherapy directly and indirectly. In addition to directly increasing cell death, high temperature increases drug entry into tumor cells and the sensitivity of tumor cells to drugs. As a result, the effect of chemotherapy applied to the peritoneum is increased.
CRS-HIPEC (hot chemotherapy) is the main treatment for pseudomyxoma peritonei and peritoneal mesothelioma. In colorectal cancers (colon cancer, rectal cancer), cure (complete recovery) is possible in selected patients.
In stomach cancer, CRS-HIPEC (hot chemotherapy) applications have been increasing in recent years. Spread to the peritoneum is common in gastric cancer, and most of the time, the peritoneum is the only site of spread. Hot chemotherapy treatment in gastric cancer should be performed in very well selected patients. The peritoneal cancer index (PCI), which indicates the extent of the disease, should be low. In other words, the disease should not have spread too much. Complete cytoreduction (CC-0) must be performed. In other words, all visible cancer foci should be removed. The patient's age, general condition and additional diseases should be taken into consideration. Otherwise, treatment cannot be successful. When appropriate patient selection is made, it is the treatment with the best results in gastric cancers that have spread to the peritoneum. Current publications indicate that cure (complete recovery) can be achieved in some patients with appropriate patient selection.
There is also the option of hot chemotherapy for ovarian cancer. Ovarian cancer is one of the most common causes of cancer-related death in women. Promising results have been obtained with hot chemotherapy in many studies. Studies on this subject are ongoing. Studies on hot chemotherapy are also being conducted in some other cancer types.
A multidisciplinary approach with surgery, medical oncology and other related departments is required in the application of hot chemotherapy. Factors such as the patient's age, general condition, comorbidities, the extent of the disease (peritoneal cancer index, PCI), the source of the disease (appendix, colon, stomach, etc.), whether the patient has received chemotherapy before, response to chemotherapy, possible side effects of the drug to be used should be taken into consideration when making a surgical decision.